Can I choose a Medicare Part D plan with better Catastrophic Coverage?
No, but you can choose a plan with lower retail drug prices.
Catastrophic Coverage cost-sharing is the same for all Medicare Part D
plans - but, Medicare plans will have different retail drug prices that
can affect your drug costs in the Catastrophic Coverage phase.
In the Catastrophic Coverage phase, you will pay the greater of a flat fee (set annually) of 5% of the plan's negotiated retail drug cost for your formulary medications, depending on the type of drug -- generics or preferred brand drugs that are multi-source drugs vs. all other drugs.
For example, in 2023, you pay the higher of either 5% of retail prices or $10.35 for brands or $4.15 for generics in Catastrophic Coverage.
So if you are using a single-source, brand drug with a $100 retail price, you would pay $10.35 since the fixed co-pay of $10.35 is more than (5% of $100) or $5. If another plan has a $150 retail cost, you would still pay $10.35 since this is still higher than (5% of $150) or $7.50. In this case retail cost does not affect your fixed Catastrophic Coverage cost.
However, for an example of a higher-costing drug: if "Medicare Part D Plan AAA" has a retail cost for Drug X of $400, you would pay $20 in the Catastrophic Coverage phase. But if "Medicare Part D Plan BBB" has a retail cost for the same Drug X of $500, you would pay $25 - or $5 more than the cost with Medicare Part D Plan AAA.
In the Catastrophic Coverage phase, you will pay the greater of a flat fee (set annually) of 5% of the plan's negotiated retail drug cost for your formulary medications, depending on the type of drug -- generics or preferred brand drugs that are multi-source drugs vs. all other drugs.
For example, in 2023, you pay the higher of either 5% of retail prices or $10.35 for brands or $4.15 for generics in Catastrophic Coverage.
So if you are using a single-source, brand drug with a $100 retail price, you would pay $10.35 since the fixed co-pay of $10.35 is more than (5% of $100) or $5. If another plan has a $150 retail cost, you would still pay $10.35 since this is still higher than (5% of $150) or $7.50. In this case retail cost does not affect your fixed Catastrophic Coverage cost.
However, for an example of a higher-costing drug: if "Medicare Part D Plan AAA" has a retail cost for Drug X of $400, you would pay $20 in the Catastrophic Coverage phase. But if "Medicare Part D Plan BBB" has a retail cost for the same Drug X of $500, you would pay $25 - or $5 more than the cost with Medicare Part D Plan AAA.
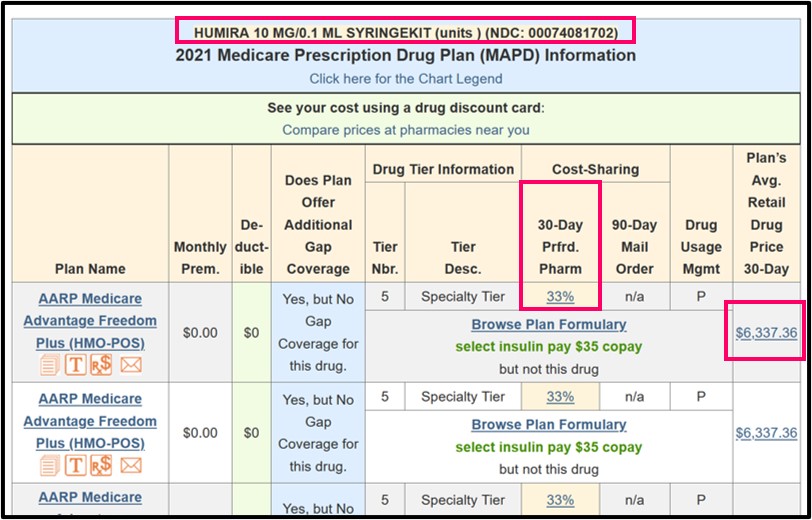
As a real-life example, a popular Medicare Part D drug with a high retail price (assume $6,000), might cost 33% of retail during the Initial Coverage Phase (about $1,980), 25% of retail in the Coverage Gap or Donut Hole ($1,500), and 5% of retail in Catastrophic Coverage ($300). If the retail cost of the medication for another Medicare Part D plan was $7,000, then you would pay $350 in Catastrophic Coverage.
As noted, if you reach the Catastrophic Coverage phase, you will find that your Medicare Part D Catastrophic Coverage phase has the same cost-sharing structure as every other Medicare Part D plan. However, your actual drug cost in this phase can vary between drug plans since your costs are based on your Medicare Part D plan's negotiated retail drug price - and retail drug prices can vary between Medicare Part D prescription drug plans.
Keep in mind that 2023 is the last year that Medicare Part D beneficiaries will pay cost-sharing in the Catastrophic Coverage phase. For plan year 2024, the Inflation Reduction Act (IRA) of 2022 eliminates beneficiary cost-sharing in the Catastrophic Coverage phase.
Browse FAQ Categories
Q1 Quick Links
- Sign-up for our Medicare Part D Newsletter.
- PDP-Facts: 2024 Medicare Part D plan Facts & Figures
- 2024 PDP-Finder: Medicare Part D (Drug Only) Plan Finder
- PDP-Compare: 2023/2024 Medicare Part D plan changes
- 2024 MA-Finder: Medicare Advantage Plan Finder
- MA plan changes 2023 to 2024
- Drug Finder: 2024 Medicare Part D drug search
- Formulary Browser: View any 2024 Medicare plan's drug list
- 2024 Browse Drugs By Letter
- Guide to 2023/2024 Mailings from CMS, Social Security and Plans
- Out-of-Pocket Cost Calculator
- Q1Medicare FAQs: Most Read and Newest Questions & Answers
- Q1Medicare News: Latest Articles
- 2025 Medicare Part D Reminder Service
